The article below was submitted by Ibex Ultrasound customer Dr. Venco of Italy.
Thoracic and Pulmonary Echotomography
Luigi Venco DMV, SCPA, EVPC Dipl.
Ospedale veterinario Città di Pavia (PV)
Cesare Rognoni, DMV
For several years, sonographers have been wrongly convinced of the impossibility to perform lung ultrasound examinations because of the acoustic impedance caused by the air inflated lungs.
Lung ultrasound examination is still a sub-utilized and scarcely known diagnostic technique even for human applications, despite veterinarian medical studies on equines (Hassel D. Thoracic Trauma in Horses. Veterinary Clinics of North America: Equine Practice, Volume 23, Issue 1, Pages 67-80) have triggered the production of a rich bibliography demonstrating the high potential of ultrasounds in pulmonary pathologies diagnosis in human beings.
Thorax radiographies is still the most utilized diagnostic instrument when dealing with pulmonary pathologies, while CT remains the “gold standard” due to the specificity and the sensibility of obtained findings.
However, it is well known that Thorax radiographs do not always provide diagnostic findings, mainly on non-cooperating or heavily dyspnoic patients and it is not always possible to obtain two adequate quality orthogonal projections.
Moreover, some intrinsic diagnostic limitations have to be added to those caused by images captured in non-ideal working conditions; thus an opaque hemithorax cannot always unequivocally be ascribed to a parenchymal or pleural disease, as well as the widespread expansion of the interstitium can be associated to several pathologies.
As previously mentioned, the pulmonary CT is the “gold standard” from a diagnostic standpoint; however its utilization in veterinarian applications is very limited by the high costs and the restricted number of equipped centers.
Pulmonary ultrasound examination does not require leading edge technological systems (the Doppler module is not strictly necessary). Transducers must include linear and 5 – 10MHz convex, depending on the animal to be analyzed.
The animal can be indifferently examined in standingl station or in sternal or lateral recumbency, without any sedation. And this represents an undisputable advantage on conventional radiology and even on CT.
For example, in absence of constraints due to patient status, dog and cat pleural effusions and pneumothorax are better evidentiated in quadrupedal station.
In order to sacn the largest possible area of the lungs surface, it is necessary to perform systematic longitudinal scanning, parallel and oblique to the ribs, on both hemi-thoraces, methodically proceeding top-down and viceversa.
Starting from the most superficial layers, different echogenicity structures are evidentiated, respectively corresponding to skin, subcutaneous tissue, muscles, ribs, parietal and visceral pleura.
Ribs cause an acoustic shadow projection which completely obscures the area underneath.
The hyperechoic line, visible in the intercostal spaces just below the ribs, corresponds to the pleural line marking the lung surface and, in normal conditions, it is constituted by the parietal and visceral components of the pleura. It looks like a less than 2mm thick regular line. Physiologically, the parietal and visceral pleura slide on each other resulting to the ultrasound investigation in a movement related to the respiratory excursions (“gliding” or “sliding”). The pleural gliding is less evident at the level of the cranic regions than at the level of the caudal dorsal ones.
Below the pleural line, the plenty-of-air lung parenchyma creates an image of amorphous with horizontal hyperechoic artifacts, called “A line”, whose mirror images repeat regularly and in depth at constant time intervals equal to the distance between skin and pleural line (Fig. 1).
Instead comet tail artifacts are extremely rare cases in normal patients and take their origin from strongly impeding spots localized in the pleura or near sub-pleura.
At the ultrasound examination, comet tail artifacts take origin from the pleural line, move following its excursions and reach the lowest part of the screen obscuring the A lines. These artefacts are called “B lines” and are caused by the edematous thickening of air surrounded interlobular septa and for such reason their presence is associated to the thickening of the interstitium (Fig. 2).
Interstitial Pattern
The interstitial pattern (parenchymal interstitial thickening or “interstitial syndrome ") is caused by the increase of extravascular liquid within the lung and can be recognized at the ultrasound scanning by the presence of multiple B lines. The presence of B lines identifies the pulmonary edema with 100% sensibility values (for humans). In practical terms, the presence of a normal ultrasound pattern (A lines) excludes the presence of a cardiogenic pulmonary edema.
The number of B lines on the pleural surface is variable, as well as the their diffusion on the two lung fields and this depends upon the severity and location of the pulmonary edema. In fact, the clinical and radiological importance of the cardiogenic pulmonary edema is strictly related to the appearing and number of B lines: they are thinning in mild cases, extended across the whole lung surface or even contiguous or confluent in severe cases.
Confluent or less-than-3mm distantiated B lines identify ground-glass areas visible at the CT scan.
The B lines are generated by the large difference of the acoustic impedance between air contained into the alveoli and interlobular pulmonary septa thickened by edema. It is well known that the pulmonary edema is visible in the radiograms only when the increase of extravascular water within the lung is at least 30% and the full-blown clinical pictures show increases superior to 75%.
Ultrasounds identify and evaluate the interstitium with much higher sensibility, earliness and simplicity than thoracic radiography and this offers substantial practical advantages in daily clinical practice.
Therefore, the presence of B lines on both the lung fields defines a damp lung. The cardiogenic pulmonary edema is the most frequent reason for that, but similar clinical pictures are observed during the acute phases of inflammatory diffuse parenchymal lung diseases, as well as in the interstitial fibrosis, and especially in the lung traumas (TLS: Traumatic Lung Syndrome).
To be noted that ultrasound pictures must be interpreted within the clinical context they are observed and, generally, this makes it easy the differential diagnosis.
When performing differential diagnosis, it is of paramount importance to be aware that the ultrasound pattern results normal in several cases, namely bronchial asthma, chronic obstructive pulmonary disease and pulmonary embolism. In these cases there is no evidence of extended thickening of the interstitium, which is instead the case for the cardiogenic pulmonary edema.
Pneumothorax
The ultrasound evidences in presence of pneumothorax (appeared the first time on literature worldwide in horse examination) are numerous, but only three of them are really important, easy to detect and have pathognomonic character:
1 Gliding (or sliding) absence,
2 Absence of B lines,
3 Presence of lung points in case of no massive pneumothorax (PNX).
As previously mentioned, parietal and visceral pleura normally slide on each other, resulting at the ultrasound investigation as a single movement related to the respiratory cycle (gliding sign).
The air interposition between the pleural leaflets prevents this movement and, consequently, the pleural line looks still. The disappearance of the gliding sign has a 100% sensibility in case of PNX diagnosis, but its specificity is between 90% and 60%. This allows to virtually exclude the PNX in case of presence, but it does not allow to guarantee the PNX in case of absence.
In fact, the pleural gliding may be absent also in case of pneumonia and atelectasis with pleural cohesion.
The B lines take their origin in the visceral pleura and are obviously absent in presence of PNX, being the pleura hidden by the air contained in the pleural cavity. The presence of just one evident B line excludes the presence of PNX even in absence of gliding sign (sensibility 100%).
The no massive PNXs show the “lung points”, which are points where the visceral pleura parietal contact appears and the PNX pattern is replaced by the normal lung pattern (gliding sign) in a well defined point moving in phase with the respiratory acts.
The lung points presence shows a 100% specificity as far as PNX diagnosis is concerned.
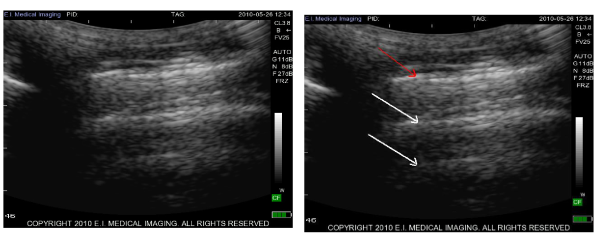
Figure 1: Gliding sign (red arrow). A lines (white arrows).
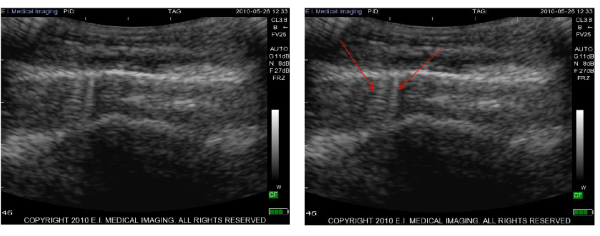
Figure 2. B lines (red arrows).
Images taken with the Ibex Pro portable ultrasound and the CL3.8 curved linear array multi frequency ultrasound transducer.
Literature
Lichtenstein DA. Rev Pneumol Clin. 2007 Apr;63(2):81-3. French.
Lichtenstein DA. Crit Care Med. 2007 May;35(5 Suppl):S262-7. Review.
Lichtenstein DA, Meziere G, Lascols N, Biderman P, Courret JP, Gepner A, Goldstein I, Tenoudji-Cohen M. Crit Care Med. 2005 Jun;33(6):1231-8.
Lichtenstein DA, Lascols N, Meziere G, Gepner A.Ultrasound in the critically ill. Intensive Care Med. 2004 Feb;30(2):276-81.
Lichtenstein DA, Lascols N, Prin S, Meziere G.Intensive Care Med. 2003 Dec;29(12):2187-92.
Lichtenstein DA, Loubieres Y.Chest. 2003 Jun;123(6):2154; author reply 2154-5.
Lichtenstein DA, Menu Y. Chest. 1995 Nov;108(5):1345-8.














